As a practicing dermatologist the commonest lymphoma that you are going to see is the T-cell lymphoma or mycosis fungoides. This condition can present initially as a patch lesion which looks for all the world like an area of dermatitis. There may be some cigarette paper thinning of the epidermis, but over time the lesion develops plaque like features and may subsequently develop tumours. None the less this progression is exceedingly slow.
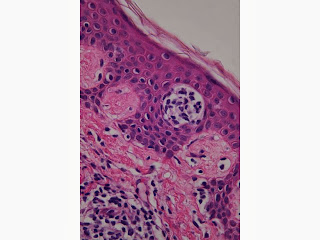
Histologically this is reflected in an initial picture of a patch stage mycosis fungoides that may show just mild spongiosis, but with an infiltrate of lymphocytes. These lymphocytes may or may not look atypical. Sometimes a useful early feature is the degree of infiltration of lymphocytes is much more than you would expect for the relatively small degree of spongiosis. Later on, the lymphocytes become more atypical and larger and may form Pautrier microabscesses, high in the epidermis. These collections of localised abnormal lymphocytes are a crucial element in making the diagnosis of T-cell lymphoma.
Mycosis Fungoides Mycosis fungoides 2
Other differentials to consider in the diagnosis of early T-cell lymphoma are just a mild dermatitis, a lichenoid drug reaction and lymphomatoid drug reaction.
An early feature of the patch test mycosis fungoides is the lymphocytes seem to line up along the dermoepidermal junction. In a lymphomatoid drug reaction there are usually more apoptotic keratinocytes.
In the plaque stage variant of mycosis fungoides you have a greater lichenoid infiltrate of lymphocytes, but in the tumour stage you will see a dense nodular infiltrate in the superficial and deep dermis and the cells look much more atypical.
There is a variant of this condition called Pagetoid Reticulosis and this is also known as the Woringer-Kolop syndrome in which there is a solitary patch or plaque usually around the lower limb or ankle. Histologically you will see the atypical large lymphocytes extensively infiltrating the epidermis and sometimes , because of the clear nature of these cells, it can even be misinterpreted as Paget's disease or even a melanoma.
Variants of T-cell lymphoma include the Folliculotrophic variant where there is extensive involvement of follicular epithelium without extensive involvement of the epidermis. You may also see follicular mucinosis. This variant often occurs on the face. When it occurs in the eyebrow area it may cause loss of the eyebrows and one has to differentiate this folliculotropic variant from follicular mucinosis which has a benign prognosis.
Another rare variant is Granulomatous slack skin disease usually presenting as thick folds of skin in the groin or axillae, but usually preceded by patches of mycosis fungoides. There is a very extensive infiltrate in the dermis and subcutaneous tissues of atypical lymphocytes but only mild epidermal involvement. Large multinucleate giant cells are sometimes seen and there is phagocytosis of the lymphocytes by these giant cells. There is extensive loss of the dermal elastic tissue fibres accounting for the folding of the skin.
Sezary's syndrome is the leukemic variant of T-cell lymphoma and usually the patient presents with erythroderma and generalised itch. There is usually extensive lymphadenopathy. The defining test is the presence of more than a 1,000 Sezary's cells per micro litre in the peripheral blood. It is important to remember that in erythrodermic Sezary's syndrome the degree of epidermal involvement may be minimal or may only show a non specific dermatitis. It is really the presence of these abnormal cells in the blood that makes the diagnosis.
Lymphomatoid Papulosis. This is divided into three types, A, B and C. In this condition papules and nodules arise in the skin and grow very rapidly but just as rapidly may necrose and involute. There may be one or many lesions on the skin usually involving the trunk or limbs. Some lesions can regress while new lesions are occurring. When a papule is histologically examined there is a wedge shaped dermal infiltrate with a mixed population of cells. When immuno-staining is done on these cells many are CD30 positive and may show Reed Stenberg like cells which have a large nucleus and prominent nucleoli.
The type B has pleomorphic lymphocytes with cerebriform nuclei and a band like infiltrate of CD30 cells and they are usually quite small lymphocytes. Epidermotropism is not a prominent feature.
In the type C there are diffuse sheets of CD30 plus cells and Reed Stenberg like cells in the dermis. Why this type of lymphoma regresses no-one really knows but presumably there is an immune attack on the cells. In about 20% of cases lymphomatoid papulosis can be associated with T-cell lymphoma or with cutaneous anaplastic large cell lymphoma or Hodgkin's lymphoma and these can precede lymphomatoid papulosis or follow it.
Occasionally you will get a T-cell lymphoma that involves the fat and this goes under the name of subcutaneous panniculitis like T-cell lymphoma. This condition can be difficult to differentiate from lupus panniculitis, but in the latter you would expect to see more damage at the basement membrane with interface vacuolisation and perhaps with some dermal mucin. A chromosome rearrangement of T-cell receptor genes is more likely to mean a subacute panniculitis like T-cell lymphoma.
The last condition I want to mention is the cutaneous gamma delta T-cell lymphoma. These patients present with large tumours particularly on the extremities and have a very rapid onset into a leukemic phase and often die.
This whole area of lymphoma diagnosis is quite difficult and has undergone radical changes in the last few years.
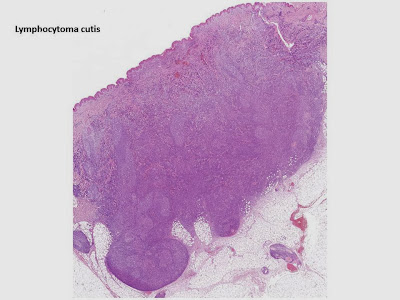
B-cell lymphomas show little in the way of epidermotropism and the abnormal cells are congregated in the dermis. The patients still generally present with red nodules or plaques, usually without any ulceration, most prominently on the head and neck, particularly in the elderly. Again these tumours tend to have a good prognosis and the first type is known as the primary cutaneous follicular centred lymphoma. It shows diffuse and nodular infiltrates in the dermis and fat with sparing of the epidermis. It may show germinal centres and have specific CD immunostains.
Primary cutaneous marginal zone lymphoma generally presents on the trunk with solitary or multiple tumours and again has a good prognosis. Again there is a lack of epidermotropism and there may be involvement of the eccrine ducts. Marginal zone lymphoma is one of the most common types of cutaneous B-cell lymphoma with five year survival rates close to 100%. They may show benign reactive lymphocytes in the centre of the lesion which may also contain germinal centres, but neoplastic lymphoid cells are found more peripherally.
The third most common type of B-cell lymphoma seen is the cutaneous diffuse large B-cell lymphoma leg type. This is generally found in elderly individuals and is more common in females. The nodules are red to brown, particularly on the distal limbs and in this case the five year survival rate is about half that of the other B-cell lymphomas, namely about 50%. In this B-cell lymphoma epidermotropism is seen and so it can simulate a T-cell lymphoma. There is a dense diffuse infiltrate of large round cell immunoblast cells in the dermis.
Pseudolymphomas
These are lesions characterised histologically by infiltrates of lymphocytes of mixed lineage ie T and B cells often with associated eosinophils. They are most commonly seen after insect bite reactions. They may show lymph follicle formation.













































No comments:
Post a Comment
Note: Only a member of this blog may post a comment.